Linking Epilepsy To Depression
October 11, 2021
There are times when sharing something in common is not good.
Depression, Anxiety, and Epilepsy are all very common disorders. Thus, it’s not surprising that these disorders coexist within one another. The brain area responsible for certain seizures can cause depression. Depression in association to epilepsy can be as high as 55 percent. And, living with epilepsy is challenging. One has to face the fear of stigma, bullying, financial problems, fear of disclosure, and the unknown of when the next seizure will happen.
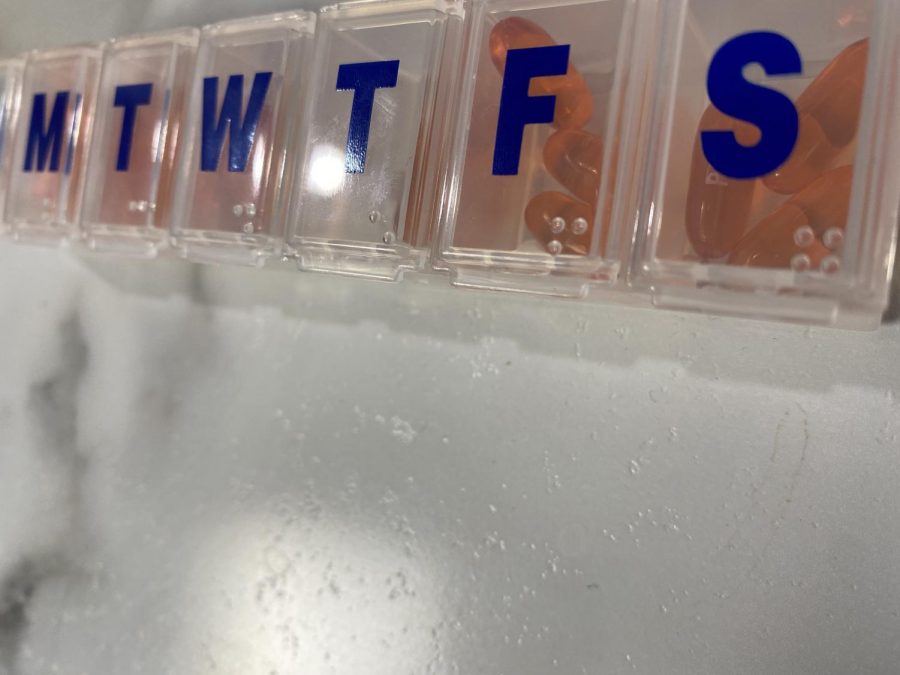
All of these examples are reasons why some people with epilepsy develop depression. Back in 2008, the FDA released a warning about how antiepileptic medicine can increase suicide and suicidal thoughts. In 2009, a study found that many other symptoms were not addressed, such as depression and anxiety. People who live with epilepsy are likely to develop depression before they know they have epilepsy or even have a seizure. This is caused by the changes in the brain that make people susceptible to seizures, which also makes them more susceptible to depression than the general population itself. When depression and epilepsy occur, it is called “comorbid.” Although epilepsy can cause depression, it’s a two-way street; depression can also cause epilepsy due to the activity in that area of the brain.
Depression can be a warning to epileptic episodes. It can evolve before people even have seizures or discover they are epileptic. Depressing thoughts and feelings are warnings that a seizure is about to occur. Knowing that depression within epilepsy can be as high as 55 percent, it is something that should not be ignored. Yet, that is exactly what occurs. Signs to look for could be lack of sleep, poor energy, no appetite, or overeating. As a parent of a former epileptic child, Elkhart teacher Andrea Holtz states, “Once my son got put on his medication, I noticed that he was more tired and caused him to lose some of his appetite.” However, Holtz noticed a benefit, as well. “Even though that was a concern, at school he started to excel in reading!”
Of the roughly 20-30 percent who have recurring episodes, 9 percent of them struggle with depression. Many studies show that uncontrolled seizures and the uncertainty of them lead to more severe forms of depression. In fact, suicide is more common with those who are epileptic than the population as a whole. Epileptic people normally have access to a large quantities of antiepileptic drugs. And, 80-90 percent of all suicide attempts (not counting the successful attempts) have been overdoses.
Although Suicide Prevention Month has come to a close, a discussion on how connected it can be to other conditions should now begin.